Signs and Symptoms of Mandible Fracture
- Pain and tenderness at the fracture site
- Changes in occlusion
- Ecchymosis of the floor of the mouth or skin
- Crepitation on manual palpation
- Soft tissue bleeding
- Sensory disturbances (numbness of the lower lip)
- Changes or deviation of the mandible on opening
- Soft tissue swelling
- Trismus
- Flexion or segmental mobility of the mandible
- Gingival tears
- Palpable fracture line intraorally or at the inferior border of the mandible
Mandible Series
- X-ray evaluation of a mandibular fracture follows a set mandibular series, which involves three views
- Posteroanterior (PA) – accurately details fractures of the ramus, angle and body
- Oblique – visualises the ramus, angle and body
- Lateral view – helpful in assessing the TMJ and any associated dislocation. A condylar fracture would also be displayed better in comparison to PA or an oblique view. Limited detail in assessing any medial or lateral displacement.
- Imaging can be supplemented further with:
- Reverse Towne’s view – Visualize the condylar region and provides detail on any medial or lateral displacement. It consists of a PA view with the patient having their cervical spine flexed and mouth open.
- Orthopantomogram (Panoramic Radiograph).
- Mandibular X-ray series. (A) Posteroanterior radiographic view of a left condylar fracture (arrow), note the obscured detail of the symphysis and condylar region due to the superimposed c-spine and mastoid process respectively; (B) left oblique view demonstrating a left angle fracture (arrow), note the normal appearance of the mandibular groove; (C) normal appearance of the mandible on a lateral projection, note how the allocated TMJ can be appreciated in this view
- Additional mandibular X-ray projections. (A) Reverse Towne’s view of a left condylar fracture (arrow), note the angle projection allows for clearer detail of the condyles due to no overlapping of the mastoid bone; (B) OPG X-ray demonstrating a left parasymphyseal fracture of the mandible (arrow); (C) OPG X-ray demonstrating a left parasymphyseal (right arrow) and right body fracture (left arrow), the segmental displacement can be appreciated in this view
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5594017/
Layers for Intraoral Surgical Access
- Posterior mandible
- Mucosa
- Submucosa
- Buccinator
- Buccopharyngeal fascia
- Periosteum
Indications for Open Reduction of Condylar Fractures
Absolute Indications
- Inability to obtain adequate occlusion using closed reduction technique
- Displacement of the condyle into the middle cranial fossa
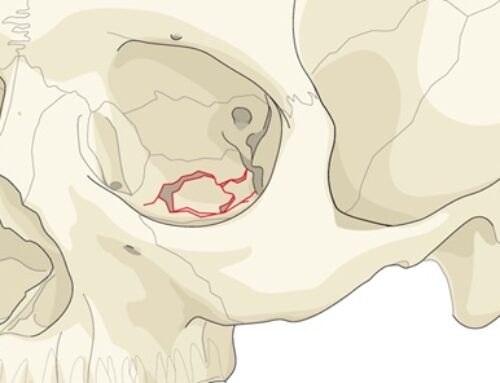
- Severe angulations of the condyle, lateral extracapsular displacement of condyle or the condyle outside the glenoid fossa
- Removal of foreign body in the joint capsule
Relative Indications
- Bilateral condylar fractures with concomitant comminuted midfacial fractures
- Bilateral fractures in an edentulous patient when splints are unavailable or impossible because of severe ridge atrophy
- Displaced condyle fracture in a medically compromised patient (e.g seizure disorder, psychiatric problems, or alcoholism) with evidence of open bite or retrusion
Submandibular Approach
Anatomic Considerations
- Marginal Mandibular Nerve – posterior to the facial artery, the marginal mandibular nerve was 1cm below the inferior border of the mandible in 19% of cases. Anterior to the facial artery, the nerve was above the inferior border of mandible (Dingman and Grabb)
- Facial Artery – runs superiorly, deep to the posterior belly of the digastric and stylohyoid muscles, and then crosses above them to descend on the medial surface of the mandible, grooving or passing through the submandibular salivary gland as it rounds the lower border of the mandible.
- Facial Vein – begins as the angular vein in the angle between the nose an eye. It runs posterior to the artery. Unlike the facial artery, the facial vein runs across the surface of the submandibular gland to end in the internal jugular vein.
Layers of Submandibular Approach
- Skin
- Subcutaneous tissue
- May see some scant superficial cervical fascia over platysma
- Platysma
- Superficial layer of deep cervical fascia
- Pterygomasseteric sling
Submandibular Approach (Risdon Approach)
- Incision 1.5-2cm inferior to the border of mandible is made through skin and subcutaneous tissue to the level of the platysma
- Use a hemostat or Metzenbaum, dissect through the platysma muscle at one end of the skin incision, undermine platysma, and push tips of the instrument back through the platysma muscle at the other end of the incision. Use scalpel to cut platysma sharply, exposing the superficial layer of deep cervical fascia
- Nick the superficial layer of deep cervical fascia and bluntly dissect with Metzenbaums or a hemostat down to periosteum
- Pterygomasseteric sling is sharply incised with a scalpel along the inferior border, which is the most avascular portion of the sling
Retromandibular Approach
Layers of Retromandibular Approach
- Skin
- Subcutaneous tissue
- Scant platysma
- Superficial musculoaponeurotic system (SMAS)
- Parotid capsule (superficial layer of the deep cervical fascia or parotideomasseteric fascia)
Retromandibular Approach (Retroparotid)
- Injection physiological solution with vasoconstrictor
- Oblique incision made through skin and subcutaneous tissue, extending from mastoid process to a point just below the angle of the mandible
- Subcutaneous tissue is undermined, exposing the superficial musculoaponeurotic system (SMAS)
- Oblique incision through the SMAS, exposing the posterior aspect of the parotid gland
- Parotid gland is lifted off masseter and retracted anteriorly
- Incision made through pterygomasseteric sling
Retromandibular Approach (Transparotid or Hinds Approach)
- Incision is made 0.5cm below the earlobe and continues 3 to 3.5 cm inferiorly just behind the posterior border of the mandible. Incision is carried through skin and subcutaneous tissues to the level of the scant platysma.
- The fusion of the platysma, SMAS, and parotid capsule are incised sharply in the vertical plane.
- Blunt dissection is begins within the gland in an anteromedial direction toward the posterior border of the mandible. A hemostat is spread open parallel to the direction of the facial nerve branches. Marginal mandibular nerve, cervical branches, and retromandibular vein may be encountered. Can dissect marginal mandibular branch from surrounding tissues proximally for 1cm and distally for 1.5-2cm.
- Pterygomasseteric sling is incised sharply in the posterior portion of the sling (bleeds less).
- Expose the mandibular angle and ramus as needed.
- Salivary cutaneous fistulae are potential sequelae to the retromandibular approach. To help avoid this complication it is recommended that a water tight closure be performed.
Pre-Auricular Approach
- The preauricular approach gives access to fractures in the mandibular condylar head and neck region. Many surgeons who perform temporomandibular joint (TMJ) surgery routinely use this incision to access the temporomandibular joint.
Anatomic Considerations in Temporal Region
Facial Nerve Trunk
- Tympanomastoid suture line is palpable as a hard ridge deep to the cartilaginous portion of the external auditory canal. The facial nerve emerges a few mm deep to its outer edge.
- Tragal pointer: facial nerve lies 1cm deep and inferior to the pointer
- Digastric muscle: during parotidectomy, lateral retraction of the SCM muscle exposes the posterior belly of the digastric. The facial nerve trunk lies 1cm above and parallel to the upper border of the digastric muscle near its insertion at the mastoid tip
Temporal Branch of Facial Nerve
The temporal branches of the facial nerve are often called the frontal branches when they reach the supraciliary region. The nerves provide motor innervation to the frontalis, to the corrugator, to the procerus, and occasionally, to a portion of the orbicularis oculi muscle. Nerve injury is revealed by the inability to raise the eyebrow or wrinkle the forehead.
The temporal branch(es) of the facial nerve leave the parotid gland immediately inferior to the zygomatic arch. It crosses superficial to the zygomatic arch deep to or within the temporoparietal fascia at an average distance of 2cm (range 0.8 cm to 3.5 cm) anterior to the anterior concavity of the external auditory canal.
- Al-Kayat and Bramley performed 56 cadaveric dissections and measured the distance from the anterior concavity of the external auditory canal to the point where the temporal branch of the facial nerve crosses the zygomatic arch. The range was found to 0.8-3-5cm with a mean distance of 20 mm.
Temporal branch of CN VII – lies immediately beneath the temporoparietal fascia above the superficial layer of the temporalis fascia.
Superficial Temporal Artery
- Superficial temporal artery – Terminal branch of external carotid artery. Divides into frontal and parietal branches a few centimeters above the arch. The superficial temporal vein and auriculotemporal nerve are posterior to the superficial temporal artery.
Pre-Auricular Approach
- Incision through skin and subcutaneous tissue is made at the junction of the facial skin with the helix of the ear. Incision includes temporoparietal fascia to the depth of the superficial layer of temporalis fascia.
- Blunt dissection with periosteal elevators and/or scissors undermines the superior portion of the incision (above the zygomatic arch). Once adequate dissection achieved, retract superficial temporal vessels and auriculotemporal nerve anteriorly. Below the zygomatic arch, blunt dissection is proceeds along the external auditory cartilage in an avascular plane between it and the glenoid lobe of the parotid gland.
- An anterosuperior incision is made through superficial layer of temporalis fascia, beginning at the root of the zygomatic arch just in front of the tragus. At the root of the zygoma, the incision is made through the superficial layer of the temporalis fascia and the periosteum of the zygomatic arch. Using a periosteal elevator beneath the superficial later of temporalis fascia, strip the periosteum off the lateral zygomatic arch. Dissection will be carried inferiorly to expose the joint capsule.
- With the condyle distracted inferiorly, pointed scissors or a scalpel is used to enter the upper joint space anteriorly along the posterior slope of the eminence. Lateral retraction allows entrance into the superior joint space.
- The inferior joint space is opened by making an incision in the disk along its lateral attachment to the condyle within the lateral recess of the upper joint space.
Rhytidectomy Approach
- Incision is made through skin and subcutaneous tissue only. Incision 1.5-2cm superior to the zygomatic arch just posterior to the anterior extent of the hairline. Incision is carried inferiorly in the natural crease anterior to the pinna (preauricular incision) and continues under the earlobe and ~3mm onto the posterior surface of the auricle instead of continuing in the mastoid-ear skin crease.
- Dissection down to bone same a retromandibular