Layers of the SCALP
The skin and subcutaneous tissue of the scalp are surgically inseparable. In addition, no easy plane of cleavage exists between the subcutaneous fat and the musculoaponeurotic layer. The aponeurosis is the true galea and has two portions, an extensive intermediate aponeurosis between the frontalis and occipitalis muscles and a lateral extension into the temporoparietal region, which is known as the temporoparietal fascia. Farther inferiorly, the temporoparietal fascia is continuous with the superficial musculoaponeurotic system (SMAS) of the face. The subgaleal fascia is the layer usually referred to as the loose areolar layer or the subaponeurotic place. This layer cleaves readily, allowing skin, subcutaneous tissue, and musculoaponeurotic layers to be stripped from the pericranium. The pericranium is the periosteum of the skull.
- Skin
- subCutaneous tissue
- Aponeurosis (galea) and muscle
- Contiguous with the Temporoparietal Fascia and SMAS
- Loose areolar tissue (subgaleal fascia)
- Periosteum (periosteum)
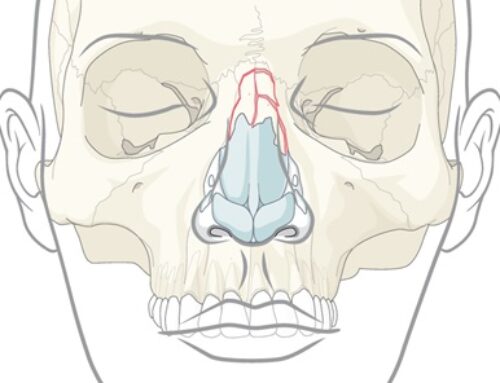
Frontal Sinus Anatomy
- Anterior table is thick (2-12 mm)
- Posterior table is thin (0.1-4 mm)
- The frontal sinus drains via a small outflow tract (frontal recess) into the ethmoid sinus/nasal cavity. The outflow tract is hour-glass shaped with the true ostium (3-4 mm) at the narrowest portion
- Frontal sinus drainage pathway – located in the posterior, inferior, and medial portion of the sinus
- Drains into middle meatus
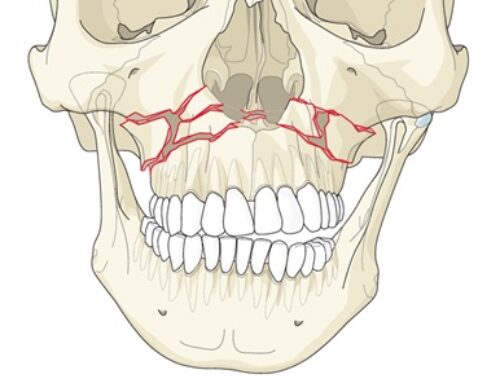
Frontal Sinus Fractures
- Frontal sinus fractures are relatively uncommon and account for only 5-10% of maxillofacial fractures
- Types of frontal sinus fx:
- Combination (anterior and posterior with or without frontal recess involvement): 2/3
- Anterior table only: 1/3
- Posterior table only: <1%
- A non-displaced posterior table fracture without CSF leak can be managed without obliteration of the frontal sinus.
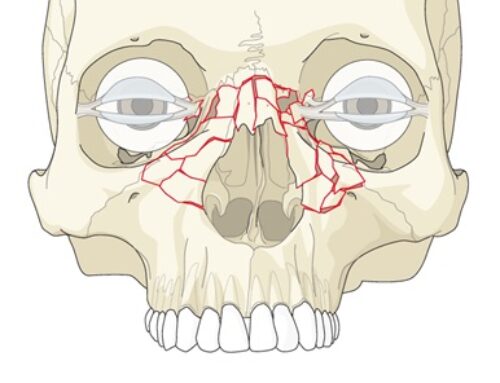
Gonty’s Classification of Frontal Sinus Fractures
- Type 1: Fractures of anterior wall
-
- Isolated anterior table
- Accompanied by supraorbital rim fracture
- Accompanied by NOE fracture
- Type 2: Anterior and posterior table fractures
-
- Linear fractures: transverse vs vertical
- Comminuted fractures: involving both tables vs accompanied by NOE fractures
- Type 3: Posterior table fractures
- Type 4: severe comminution of whole frontal area, involving the orbit, the nasal bone and the ethmoid
Indications for Obliterating Frontal Sinus
- Occlusion of the nasofrontal ducts requires removal of all sinus mucosa from the frontal sinus, inversion of the mucosa into the ducts, and elimination of dead space. This eliminates the possibility of developing a hematoma or seroma.
- Fat has been historically used.
- Calcium phosphate bone cement is a near ideal alloplast in that it has unlimited availability, is biocompatible, has high mechanical strength, has a low risk for infection, is radiopaque and is incorporated into the bone. It does have drawbacks. It is expensive, and when placed directly over dura or sinus membranes, it breaks up and a chronic foreign body reaction ensues.
Indications for Cranialization
- CSF leak
- Frontal craniotomy
- Posterior table removal
- Dural tear repair
Frontal Sinus Exam & Assessment
- Evaluation for any contour deformity – aesthetics
- Frontal laceration
- Neurosensory deficits
- CSF leak: check for presence of clear nasal drainage or posterior nasal drainage that might be indicative of a CSF leak.
- Examination of deep wounds should be performed under sterile technique, as these can be through and through injuries. The prognosis for such severe injuries is significantly worse and more aggressive management is indicated.
- A high resolution CT scan with axial, coronal, sagittal and 3-D reconstruction is the gold standard for diagnosis.
CSF Leak
Otorrhea or rhinorrhea suspected of CSF leak
- Halo Sign Test
- Bloody rhinorrhea suspicious for CSF can be placed on filter paper and observed for a halo sign. If CSF present, it diffuses faster than blood and results in a clear halo around the central stain.
β2 transferrin
- B2 transferrin is one of two major variants of iron binding transferring glycoproteins. It lacks a carbohydrate side chain which increases its positive charge, permitting isolation during electrophoresis. B2 transferrin is only found in cerebrospinal fluid, aqueous humor, and perilymph. Thus, with the exception of a ruptured globe, it is an ideal substance to distinguish between cerebrospinal fluid, nasal secretions and serum.
- Found in cerebrospinal fluid, vitreous humor of eye, perilymph
- False positive when sample contaminated by ruptured globe
- Iron binding transferrin glycoprotein; lack carbohydrate side chain, increasing net positive charge
Glucose exam
- Imaging – CT cisternogram after administration of inthrathecal fluorescein
Complications of Frontal Sinus Fractures
- Most common early complication – Meningitis
Most common chronic complication – Mucocele - Early
- Meningitis
- Late
- Mucocele
- Mucopyocele
- Post surgical
- Visible scar
- Paraesthesia
- Alopecia
- Brow ptosis
- Other: pneumocephalus
Technique of Coronal Approach
- Hemostatic agent i injected into the subgaleal plane to promote hemostasis and to help separate the tissue layer.
- Incision on the scalp is made through skin, subcutaneous tissue, and galea 4 to 5 cm within the hairline, revealing the subgaleal plan or loose areolar connective tissue overlying the pericranium.
- After elevation of the anterior and posterior wound margins, hemostatic clips (Raney clips) may be applied.
- Subgaleal dissection is carried anteriorly until a point 3 to 4 cm superior to the supraorbital rims. A horizontal incision is made through the pericranium from one superior temporal line to the next.
- Depending on amount of exposure required, coronal incision can be carried inferiorly to the helix (if exposure of zygomatic arch is not necessary) or to the level of the earlobe as a preauricular incision (allows exposure of zygomatic arch, temporomandibular joint, and infraorbital rims)
- Skin incision below the superior temporal lines should extend to the depth of the superficial layer of the temporalis fascia.
- Once the lateral portion of the flap has been elevated to within 2 to 4 cm of the body of the zygoma, the flap is dissected inferiorly to the root of the zygomatic arch.
- Incision of the superficial layer of temporalis fascia is made anteriorly and superiorly at a 45⁰ angle, joining the cross-forehead incision made at the pericranium at the superior temporal lines.
- Dissection is carried down to the zygoma and periosteum is incised sharply over zygomatic arch.
- It may be necessary to release the supraorbital neurovascular bundle from its notch or foramen by using a osteotome to remove the bon bridge along the supraorbital rim
- The medial canthal tendons should not be inadvertently stripped. The anterior and posterior ethmoid arteries can be cauterize. With a periosteal on each side of the foramen, retraction allows the periosteum attached to the foramen to tent outward to allow for cauterization of the vessels.
- The inferior edge of the superficial layer of the temporalis fascia is sutured 1 cm superior to the superior edge of the incised fascia. The scalp is closed in two layers. Slow resorbing 2-0 sutures are used to reapproximate the galea/subcutaneous tissue. A suction drain (usually 7 mm flat) can be placed before suturing the skin with 2-0 resorbing or permanent sutures.